To operate or not to operate?
Prioritising your surgical waiting list
The impact of coronavirus is now embedded into our ways of working and how we deliver healthcare services. As trusts continue to manage the reducing number of cases, the focus is now on reinforcing cancer and urgent surgery and restarting elective surgery services, be that at local trust level or using capacity across a system footprint.
Surgical services need to restart at pace and it may be tempting to revert to how things were before – to allocate a specific number of lists to each speciality for them to fill based on their own criteria. However, as waiting lists have been growing and capacity is not yet back to pre-pandemic levels and it may not be for some time to come, this method comes with added risk. How do you ensure that each patient on the waiting list is treated fairly? How do you ensure one speciality or patient group is not neglected over another widening inequalities? More importantly, how can we make decisions to ensure that we are directing our resources to those patients that need them the most?
Attain’s Surgical Prioritisation Framework
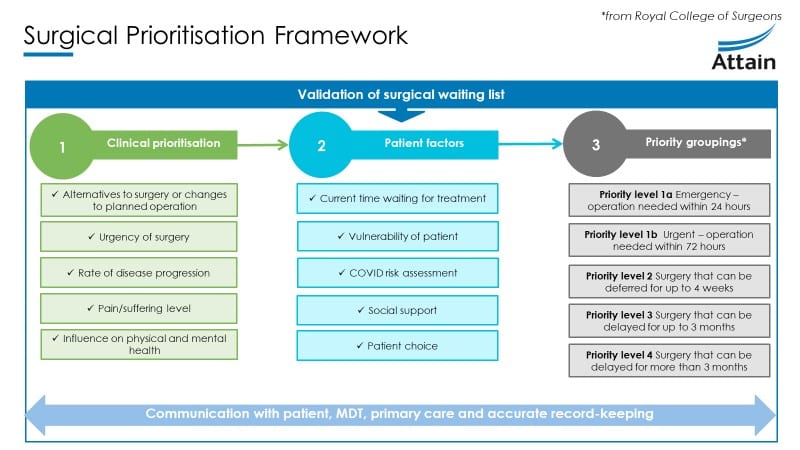
Patients will now need to be prioritised through a clinically led, robust prioritisation framework. This framework can be used for all patients on a surgical waiting list – cancer, urgent, elective or all three. More specific guidelines for obstetrics and gynaecology, transplantation and cancer planning services are available. There are three main factors that will need to be considered when prioritising your patients:
Clinical prioritisation
Patient factors
Priority groupings
Creating sufficient capacity
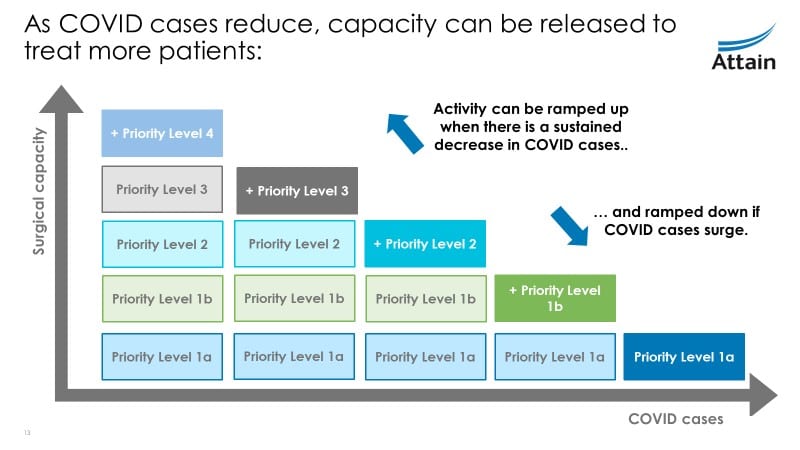
Once patients have been assessed and grouped into priority levels, the number of priority groups that are able to be operated on depends on viral load, local and system capacity and resource availability.
An assessment of sufficient capacity should include:
- Current viral load in the environment
- Diagnostic capacity
- Number and skill-mix of workforce
- Pre-assessment, theatre, recovery and post-operative capacity
- Supplies and surgical equipment
- COVID testing, infection control and PPE requirements
If local capacity is not sufficient, organisations should consider regional surgical networks to fulfil requirements. In the current climate, it is necessary to be agile with our capacity, and be able to ramp it up or down responding to wider determinants like COVID.
Success factors
Prioritisation of your entire waiting list may seem daunting but Attain are extensively experienced in developing automated tools to help make this easier, demand and capacity simulations as well as developing the governance needed to wrap around such a process. We have found that the critical factors leading to a successful prioritisation are clinical leadership, clear documented communication between all parties involved and an accurate record of prioritisation outcomes so that patients don’t get lost in the system.
If you would like to start thinking about best practice and discuss how you can optimise the prioritisation processes within your organisation or system, please do not hesitate to get in touch with Dr Vineeta Mann on vineeta.mann@attain.co.uk for more information.
Our Acute Projects
Contact us to discuss your challenges
Get in touch with us to learn more about how we can support you in addressing your challenges.
Complete our simple form and we’ll call you right back, alternatively just email: