A ‘Hub’ approach can improve quality, integrate care, and increase capacity
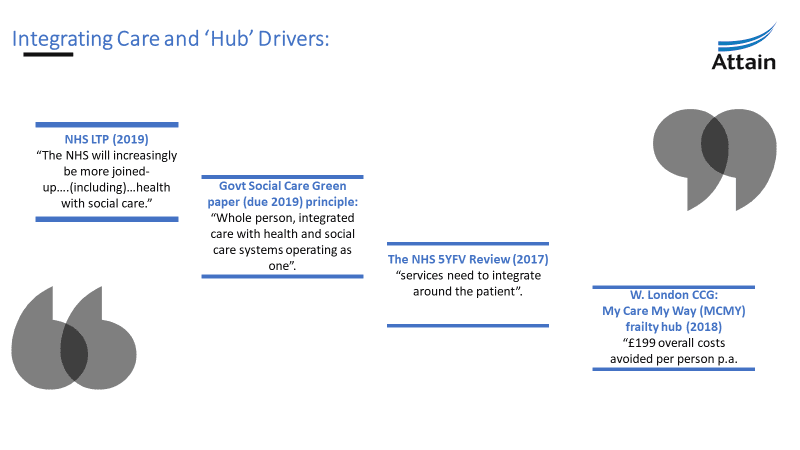
Both the NHS Long Term Plan (2019) and the overdue government green paper on social care reflect integrated care as key to managing growing demand and improving patient access. Good models of integrated care will include prevention, self-care and social prescribing, as well as traditional health and social care services. Systems are increasingly looking towards care hubs as a tried and tested way to implement integrated models of care.
In this article, Norma Christison and Su Gordon-Graham explore the rationale for developing integrated care hubs and the key ingredients for successful implementation.
Traditional models versus integrated ‘Hub’ models
Traditional medical models of care and silo working no longer meet increasing demand and is impacted by limited resources – funding, staff, estates and poor access to shared patient records.
The future delivery of care must change if it is to deliver high quality, safe and timely care that is affordable and meets patient need. This is particularly true for the UK’s aging population, many of whom have multiple long-term conditions that require complex management. These may be better met by developing new roles and models of care that are joined-up and seamlessly delivered in partnership with the patient across care providers and voluntary services.
Attain has direct experience in designing and implementing both physical and virtual hubs to deliver integrated, coordinated, seamless care.
The ‘Hub’ model is an increasingly well evidenced, attractive option that aims to reduce duplication across the system and improve patient flow.
Integrated models of care have been shown to be effective. NHS England (NHSE) tested the Five Year Forward View models of care over three years at Vanguard sites from 2015-2018; and reported a “statistically significant reduction in emergency admission rates for Vanguard sites, at 1.6%, compared to other NHS sites (3.1%)”. [1]
Developing a ‘Hub’ model of care provides an opportunity to create new and ‘blended’ health and social care roles to support delivery. Hubs allow you to extend or to create joint roles to reduce duplication in the system and delayer services, making them easier for patients to negotiate by sharing patient information (assessment) and supporting joint care planning across services. It is important for systems to partner-up with their local university or academic institution in order to provide training, professional accreditation and a structured career pathway for staff taking on new roles.
Attain has supported the design, development, and effective implementation of integrated care ‘Hub’ models in several Sustainability and Transformation Partnerships (STPs)/Integrated Care Systems (ICS) and Clinical Commissioning Groups (CCGs); including the West London CCG’s pioneering frailty ‘Hub’ that also created some of the new roles discussed above.
[1] The NHS Long Term Plan, Figure 1, NHS England, 8 January 2019
Use a ‘Hub’ implementation framework
The Attain ‘Hub’ implementation framework is an effective method to develop an integrated care ‘Hub’.

The five key ingredients to getting started:
- Articulate what your local issues are that a ‘Hub’ is trying to solve. Discuss individual organisational and collective issues in a collaborative forum and analyse population and health management data to identify local issues i.e. quality of care, a lack of capacity, increasing or uncontrolled demand, affordability, or the need to reduce avoidable and/or duplicated costs?
- Agree the service/care model you are trying to implement. If there is no model, work with partners to develop one. Identify the patient cohort and services that the ‘Hub’ will provide and ensure clear understanding by all stakeholders.
- Decide what type of ‘Hub’ you need. This will be based on the ‘issues’ and the service model (above) and work within known constraints to design and deliver it i.e. resource, affordability and consensus. Potential ‘Hub’ types include: a physical building that co-locates services/staff, or a lower cost ‘Hub’ model that can be delivered within existing estates (a central GP Practice or Community service setting). These can typically be a single long-term condition (LTC) ‘Hub’ clinic for a cluster population, or a ‘virtual’ single point of access-type ‘Hub’ that co-ordinates referrals – typical of some Vanguard frailty ‘Hub’ models that used a case co-ordinator approach to join-up care.
- Identify funding, budget and resource. Establish the resources already available in the system and the gaps i.e. funding, workforce (roles, capacity, ways of working), protocols, indemnity, estates, IT kit, systems and infrastructure required. Work together to pool or procure required resources, and/or to develop and recruit to new roles.
- Identify new ways of working, governance and joint working arrangements/structures. This will include collaborative leadership, vision, and levels of responsibility. Generate aligned policies, decision-making protocols, agreed principles of working together, information-sharing agreements, and develop standing operating procedures to deliver the agreed service model. Agree the preferred finance model such as an outcomes-based, risk-sharing approach to ensure co-operation , engagement, and aligned incentives across the integrated system.
Whilst the core elements to developing integrated ‘Hub’ models of care may require a change in the way services are commissioned, their associated contractual arrangements and the way in which organisations work together, the true impact of integration is reliant solely on the ability of frontline staff and managers to make it work.
If you need help developing an integrated model of care, please contact Gareth Hartley directly.
References:
- The NHS Long Term Plan, NHS England, 8 January 2019
- Briefing Paper 8002, Social care: forthcoming Green Paper (England), House of Commons, 13 May 2019. Tim Jarrett
- Next steps on the five year forward view, page 32, NHS England, March 2017
- Evaluation of My Care My Way, W. London CCG: summary findings, Buckinghamshire University, January 2018, doctors S. Proctor and D. Hancock.
- Better Local Care MCP Vanguard: Synthesis of Year 1 evaluation evidence (2016 – 2017), RSM UK, July 2017.
- https://attain.co.uk
Contact us to discuss your challenges
Get in touch with us to learn more about how we can support you in addressing your challenges.
Complete our simple form and we’ll call you right back, alternatively just email: