Attain’s Impact on Diagnostic Tests in England
Attain’s huge impact on diagnostic tests in England. 1 in 12 new diagnostic tests are in Community Diagnostic Centre facilities that Attain helped set up – from business case and design through to delivery. We have been the delivery partner to the NHS to ensure timely implementation that impacts patients and services alike. For example, […]
Population Health Management: A robust approach to understand and plan for COVID-related inequalities
COVID has exposed previously hidden inequalities
As we have discussed previously, COVID has laid bare societal inequalities in the UK. Public Health England (PHE) has highlighted a number of areas of disparities in COVID rates and outcomes including age, deprivation, comorbidities and ethnicity. This list represents a mix of some COVID specific biological risk factors but is predominantly driven by social inequalities.
Consideration must be given as to how the widening of inequalities may be mitigated against over the medium and long-term. The pandemic has disproportionately affected several population groups and establishing a population health approach at place has been identified as a way forward in terms of recovery and renewal from the pandemic. There is now a timely opportunity to really focus on understanding population health and implement PHM to address inequalities.
To begin to plan responses and services for these groups within a population, we need to understand how many people of each group there are, together with recent basic demographic data. The absence of this data has hampered local response efforts and continues to slow planning for a second wave of COVID-19 and beyond. In order to better coordinate a response to future outbreaks, we need to make sure we gather and analyse data on our populations. The data required to report on these areas going forward should be available on a person level and be as recent as possible – this data forms a cornerstone of a PHM based response to COVID-19.
What is needed to deliver PHM based risk stratification for COVID?
- COVID specific patient segmentation model: This defines our sub-populations and gives an outline of data that is required. The choice of risk factors may need to reflect the available data, recognising that time is short to collect new data metrics. This should be augmented with COVID-19 history if available (i.e. antibody test results).
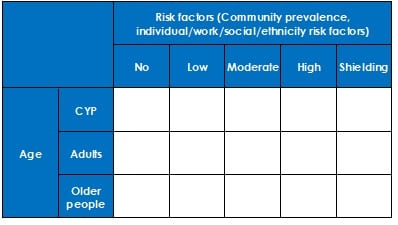
- Patient level data: To complete segmentation analysis, either GP data or similar data including risk factors, social prevalence, ethnicity, deprivation, presence of mental health conditions, social vulnerability, LTCs
- Plan of action for each segment: Ranging from whole population messaging through to personalised care coordination.
- Plan to update this model: As new information and guidance becomes available
Where should this function sit?
This all needs to be owned by a joined up, system wide analytics team that can feed the relevant data to the relevant providers. These teams should have access to recent data and permission to use and share it rapidly
How should this new intelligence be used?
This information should be reported regularly to health planning elements of systems, primary care providers and other health system partners as part of a PHM risk identification process to allow rapid assessment of who needs what. We don’t need perfect health system data to make a start with PHM – simple, person level demographic data is extremely useful in planning for future waves. We can add in health system and other relevant data, where available and appropriate.
What is the planned impact of this approach?
Combined with effective integrated commissioning – that seeks to make the biggest impact with collective resources – PHM can help to nurture collaboration across health and care to address wider issues linked to poverty and social exclusion, taking an evidence-based approach to tackling the wider determinants of health and working with the VCS to co-ordinate support for vulnerable residents and communities most affected. As Integrated Care Partnerships (ICPs) emerge, with providers potentially playing a bigger role in commissioning decisions, Integrated Care Systems can design strategies to deliver place-based PHM.
How can Attain support you?
Our PHM and analytics experts have experience of developing and implementing PHM strategies with places and systems, including segmentation model development, data sourcing and the associated service transformation. Our current project work includes reviews of PHM-linked outcomes frameworks for children and young people in the North of England and older people in London.
Please contact Matt Jones via contacts@attain.co.uk to understand how we can help you put this into practice.
Contact us to discuss your challenges
Get in touch with us to learn more about how we can support you in addressing your challenges.
Complete our simple form and we’ll call you right back, alternatively just email: